
Efficiently Verify Primary and Secondary Coverage Details, such as Member ID, Group ID, Coverage Period, Co-Pay, Deductibles, and Co-Insurance and Benefits Information.

Your patients’ information is safe with us as we’ve ensured our services are HIPAA compliant throughout the process

Credentialing of your practice by the payor is also offered, along with prior insurer approval before a claims submission.

Charges for Medical Services and other Patient-Facing Services are submitted to the appropriate payors for billing.

Claims are submitted electronically through the practice management system, ensuring quick and reliable communication and outcomes.

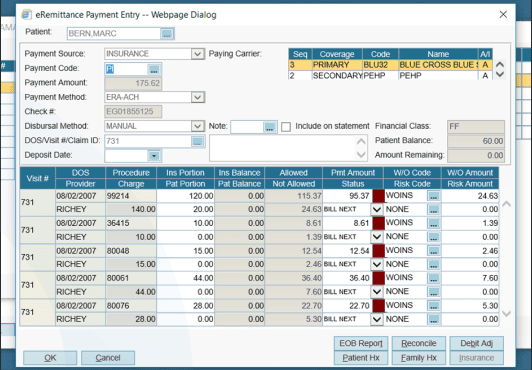
Remittance advice, Patient Payment, and Explanation of Benefits (or EOB’s) are received by us, along with payment from insurance agencies.

Careful inspection of Account Receivable balances, and separation of accounts as collectible and non-collectible.

Classification of denials under various factors to simplify the process, and develop strategies specific to your practice.
Good practices dictate denied claims are bad for business, and part of having your claims pass the insurer is to identify common problems faced by customers to better assist them in getting their claims passed.


Creating a user account using patient’s demographic and insurance information

Verify that the patient's insurance plan covers the services being requested

Obtaining prior approval from an insurance company before providing certain medical services

Entering the services’ charges into the medical practice’s billing software

Submitting the claims to the insurance companies for payment

Updating the medical practice’s billing system with the payments received from insurance companies and the patient

Any denied claims are resubmitted, as the insurer could have denied a claim for non-insurance related reasons

Following up with the insurer to clear any unpaid claims.

Collecting payment for any outstanding balances from patients

Determining areas for improvement by generating reports that track the financial performance of the medical practice

Claims Settlement
MDsure offers many benefits over traditional methods of claims management, more importantly, it takes the load off hospitals and allows them to function smoothly and without the hassles of dealing with the finances.
The peace of mind working with MDsure brings me with regards to my practice and financial security is priceless.
MD Neurologist
If you’re a doctor who is looking to outsource your medical billing, I highly recommend reaching out to a reputable company. It’s a great way to save time and money, and it will allow you to focus on what you do best: providing care for your patients.
MD
As a busy medical practitioner, I can confidently say that partnering with MDsure has been a game-changer for my practice. Their expertise in medical billing and coding has streamlined our revenue cycle management, ensuring that we get paid accurately and promptly for the services we provide.
PharmD, BCOP
Their team’s attention to detail, compliance knowledge, and commitment to staying up-to-date with industry changes have taken a huge burden off my shoulders.
MD
I can now focus on what truly matters – providing quality patient care – while knowing that our financial processes are in capable hands.
MD
I’m so much happier now that I don’t have to worry about medical billing. I would highly recommend outsourcing your billing to a third-party company if you’re a doctor.
MD
MDsure can be tailored to your specific needs and provide affordable and effective ways to manage your customers, while simultaneously reducing costs and maximizing profits. Let us know you’re interested and an MDsure agent will assist you with your queries shortly.